Cyclobenzaprine hydrochloride (a prescription-only medication known as Flexeril) is a central nervous system muscle relaxant designed to relieve pain and discomfort related to muscle spasms, sprains and other muscle injuries. It is usually used in conjunction with rest, physical therapy and other measures.
Cyclobenzaprine is not designed for long-term use, and patients should follow the regimen provided by their physician, said Dr. Kiran Patel, pain management specialist at Lenox Hill Hospital. “It’s a muscle relaxant that can help with a muscle spam or the sensation of tightness,” Patel told Live Science.
Cyclobenzaprine is often prescribed to people who have acute back injuries, including when people report having muscle spasms or significant tightness in their back, or when the back feels like it’s locked, she explained. It’s also prescribed to treat for muscle strains.
Cyclobenzaprine is used short-term to treat muscle spasms. It is usually used along with rest and physical therapy. It works by helping to relax the muscles.Flexeril (cyclobenzaprine) is a muscle relaxant. It works by blocking nerve impulses (or pain sensations) that are sent to your brain.
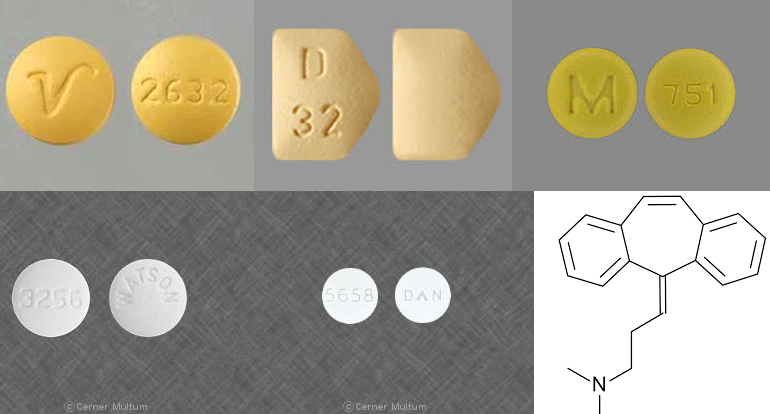
Cyclobenzaprine, a centrally-acting muscle relaxant, was first synthesized in 1961 and has been available for human use since 1977. It was initially studied for use as antidepressant given its structural similarity to tricyclic antidepressants – it differs from Amitriptyline by only a single double bond. Since its approval, it has remained relatively popular as an adjunctive, short-term treatment for acute skeletal muscle spasms secondary to musculoskeletal injury.
Flexeril is used together with rest and physical therapy to treat skeletal muscle conditions such as pain, injury, or spasms.
Cyclobenzaprine is a muscle relaxant. It works by blocking nerve impulses (or pain sensations) that are sent to your brain. Cyclobenzaprine is used together with rest and physical therapy to treat skeletal muscle conditions such as pain or injury. Cyclobenzaprine may also be used for purposes not listed in this medication guide.
How to use Cyclobenzaprine Tablet
Generic Flexeril (cyclobenzaprine) is a muscle relaxer that relieves pain and discomfort caused by strains, sprains, and other muscle injuries. Flexeril is commonly prescribed for short-term use, in combination with rest and physical therapy, after accidents or other circumstances where healing may be slowed by muscle strain. In some cases, Flexeril can be used to treat pain from certain musculoskeletal disorders like fibromyalgia. Flexeril is chemically related to a class of antidepressants called tricyclic antidepressants, and works by acting on the central nervous system, blocking nerve impulses (or pain sensations) that are sent from sore muscles to the brain.
Take this medication by mouth with or without food as directed by your doctor. Do not increase your dose or use this drug more often or for longer than prescribed. Your condition will not improve any faster, and your risk of side effects will increase.
The dosage is based on your medical condition and response to treatment. This medication should only be used short-term (for 3 weeks or less) unless directed by your doctor.
Tell your doctor if your condition persists after 2 to 3 weeks or if it worsens.
The mechanism of action of cyclobenzaprine
The exact mechanism of action of cyclobenzaprine has not been fully elucidated in humans, and much of the information available regarding its mechanism has been ascertained from early animal studies. There is some evidence that cyclobenzaprine exerts its effects at the supraspinal level, specifically within the locus coeruleus of the brainstem, with little-to-no action at neuromuscular junctions or directly on skeletal musculature.
Action on the brainstem is thought to result in diminished activity of efferent alpha and gamma motor neurons, likely mediated by inhibition of coeruleus-spinal or reticulospinal pathways, and ultimately depressed spinal cord interneuron activity.
More recently it has been suggested that inhibition of descending serotonergic pathways in the spinal cord via action on 5-HT2 receptors may contribute to cyclobenzaprine’s observed effects.
Cyclobenzaprine is extensively metabolized in the liver via both oxidative and conjugative pathways. Oxidative metabolism, mainly N-demethylation, is catalyzed primarily by CYP3A4 and CYP1A2 (with CYP2D6 implicated to a lesser extent) and is responsible for the major metabolite desmethylcyclobenzaprine. Cyclobenzaprine also undergoes N-glucuronidation in the liver catalyzed by UGT1A4 and UGT2B10, and has been shown to undergo enterohepatic circulation.
Cyclobenzaprine is a tricyclic amine salt that works in the central nervous system (CNS) as a depressant and sedative and has associated effects of reducing muscle hyperactivity. It has FDA-approval as an adjunct to rest for the treatment of muscle spasm associated with acute, painful musculoskeletal conditions. Cyclobenzaprine is a centrally-acting muscle relaxant that reduces tonic somatic motor activity, which may influence alpha and gamma motor neurons at the level of the spinal cord
Important Information
You should not use cyclobenzaprine if you have an allergy to the medication, a certain type of thyroid disorder (hyperthyroidism), heart block, congestive heart failure, a heart rhythm disorder, or you have recently had a heart attack.
Do not use cyclobenzaprine if you have taken an MAO inhibitor in the past 14 days, such as isocarboxazid, linezolid, phenelzine, rasagiline, selegiline, or tranylcypromine.
Before taking this medicine
You should not use cyclobenzaprine if you are allergic to it, or if you have:
- hyperthyroidism;
- heart block, heart rhythm disorder, congestive heart failure; or
- if you have recently had a heart attack.
Cyclobenzaprine is not approved for use by anyone younger than 15 years old.
Do not use cyclobenzaprine if you have taken an MAO inhibitor in the past 14 days. A dangerous drug interaction could occur. MAO inhibitors include isocarboxazid, linezolid, phenelzine, rasagiline, selegiline, and tranylcypromine.
Some medicines can interact with cyclobenzaprine and cause a serious condition called serotonin syndrome. Be sure your doctor knows if you also take stimulant medicine, opioid medicine, herbal products, or medicine for depression, mental illness, Parkinson’s disease, migraine headaches, serious infections, or prevention of nausea and vomiting. Ask your doctor before making any changes in how or when you take your medications.
To make sure cyclobenzaprine is safe for you, tell your doctor if you have:
-
-
- thyroid disease;
- liver disease;
- glaucoma;
- enlarged prostate; or
- problems with urination.
-
It is not known whether cyclobenzaprine will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
It may not be safe to breast-feed while using this medicine. Ask your doctor about any risk.
Older adults may be more sensitive to the effects of this medicine.
Cyclobenzaprine is usually taken taken for up to 2 or 3 weeks. Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose.
Follow your doctor’s dosing instructions very carefully.
Swallow the capsule whole and do not crush, chew, break, or open it.
Call your doctor if your symptoms do not improve after 3 weeks, or if they get worse.
Store at room temperature away from moisture, heat, and light.
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. An overdose of cyclobenzaprine can be fatal.
Overdose symptoms may include severe drowsiness, vomiting, fast heartbeats, tremors, agitation, or hallucinations.
What should I avoid while taking cyclobenzaprine?
Avoid driving or hazardous activity until you know how this medicine will affect you. Your reactions could be impaired.
Avoid drinking alcohol. Dangerous side effects could occur.
Cyclobenzaprine side effects
Get emergency medical help if you have signs of an allergic reaction to cyclobenzaprine: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Stop using this medicine and call your doctor at once if you have:
-
-
- fast or irregular heartbeats;
- chest pain or pressure, pain spreading to your jaw or shoulder; or
- sudden numbness or weakness (especially on one side of the body), slurred speech, balance problems.
-
Seek medical attention right away if you have symptoms of serotonin syndrome, such as: agitation, hallucinations, fever, sweating, shivering, fast heart rate, muscle stiffness, twitching, loss of coordination, nausea, vomiting, or diarrhea.
Serious side effects may be more likely in older adults.
Common cyclobenzaprine side effects may include:
-
-
- drowsiness, tiredness;
- headache, dizziness;
- dry mouth; or
- upset stomach, nausea, constipation.
-
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Toxicity
Cyclobenzaprine is structurally similar to amitriptyline and only differs in a double bond in the central amine ring. Due to its structure, cyclobenzaprine is structurally and pharmacologically related to the tricyclic antidepressants. In theory, it should pose similar toxicities to tricyclic antidepressants; however, retrospective studies that have looked at reported cyclobenzaprine overdoses are conflicting. Among the most feared toxicities associated with cyclical antidepressants, overdoses are their effects on fast-acting sodium channels in the cardiac conduction system.
Cyclical antidepressants block the cardiac sodium channel and cause prolongation of cardiac depolarization, which manifests as QRS widening on electrocardiograms. There is also evidence that cyclical antidepressants may decrease the seizure threshold by interfering with chloride conductance on the GABA receptor.
Some case reports show that cyclobenzaprine overdoses have fatal tendencies. Other retrospective studies show that their toxicities may manifest slightly differently than other tricyclic antidepressant medications. These particular studies indicate the theoretical risks that are associated with traditional tricyclic antidepressants, such as cardiac dysrhythmias from a widening of the QRS complex due to sodium channel blockade, and seizures may not apply to cyclobenzaprine toxicity despite their similarities in chemical structures.
In one retrospective review comparing isolated ingestions of cyclobenzaprine to its sister drug amitryptiline, the authors found that the cyclobenzaprine overdoses resulted in no deaths, no ventricular dysrhythmias, and reduced numbers of seizures as compared to the cases of amitryptiline overdoses in the same period.
The authors, therefore, concluded that despite being a tricyclic antidepressant in its structure, cyclobenzaprine correlates with less incidence of tricyclic antidepressant-like complications when compared to amitryptiline.
One study retrospectively looked at 750 charts at five regional poison centers between the years of 1989 to 1993. Out of the 750 charts, 523 had sufficient data for review. Out of these, 402 were reportedly pure cyclobenzaprine ingestions, and 121 were multidrug overdoses. No one case exceeded 1000 mg of cyclobenzaprine in the ingested dose. The chart reviews reported no seizure activity.
Dysrhythmias beyond sinus tachycardia were infrequent, and none were found to be life-threatening. No deaths occurred. These findings are different from the theoretical neurotoxic and cardiotoxic effects seen with traditional tricyclic antidepressant overdoses in which seizures and dysrhythmias are often life-threatening.
The authors concluded that based on their retrospective study, cyclobenzaprine in toxic doses less than 1000 mg does not appear to produce the life-threatening neurotoxicity and cardiotoxic dysrhythmias associated with traditional tricyclic antidepressants.
Other case reports, however, have implicated cyclobenzaprine in acute overdose as the culprit leading to fatalities. In one case report, there were two reported two cases of overdoses in which elevated levels of cyclobenzaprine were found in postmortem evaluations of the patients.
Although it is unknown the exact mechanism by which the fatalities occurred (i.e., dysrhythmias, seizure activity), blood samples revealed elevated levels in both patients that suffered deaths. Estimates by the author put these levels equivalent to approximately 800 mg of cyclobenzaprine. The authors, therefore, document an association linking elevated cyclobenzaprine levels with two examples of presumed fatal overdoses.
Cyclobenzaprine may interact with other medications
Cyclobenzaprine oral tablet can interact with other medications, vitamins, or herbs you may be taking. An interaction is when a substance changes the way a drug works. This can be harmful or prevent the drug from working well.
To help avoid interactions, your doctor should manage all of your medications carefully. Be sure to tell your doctor about all medications, vitamins, or herbs you’re taking. To find out how this drug might interact with something else you’re taking, talk to your doctor or pharmacist.
Examples of drugs that can cause interactions with cyclobenzaprine are listed below.
Drugs you should not take with cyclobenzaprine
Do not take monoamine oxidase inhibitors (MAOIs) with cyclobenzaprine. Doing so can cause dangerous effects in the body. Examples of these drugs include:
- selegiline
- rasagiline
- tranylcypromine
Taking this drug with an MAOI or within 14 days of stopping an MAOI could increase your risk of serious side effects. These include seizures.
Interactions that increase your risk of side effects
Taking cyclobenzaprine with certain medications raises your risk of side effects from cyclobenzaprine. This is because the amount of cyclobenzaprine in your body is increased. Examples of these drugs include:
- Benzodiazepines, such as triazolam, alprazolam, and midazolam. You may have more sedation and drowsiness.
- Barbiturates, such as phenobarbital. You may have more sedation and drowsiness.
- Certain drugs used to treat depression, such as fluoxetine, venlafaxine, amitriptyline, or bupropion. You may be at a greater risk for serotonin syndrome.
- Verapamil. You may be at a greater risk for serotonin syndrome.
- Anticholinergic drugs, such as tolterodine or oxybutynin. You may be at a greater risk for certain side effects. These include dry mouth or not being able to urinate.
Interactions that can make your drugs less effective
When certain drugs are used with cyclobenzaprine, they may not work as well. An example of these drugs includes guanethidine. Cyclobenzaprine can block the blood pressure-lowering effect of guanethidine. This means your blood pressure may increase.
This list is not complete. Other drugs may interact with cyclobenzaprine, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Cyclobenzaprine Manufacturers
-
-
- Anesta ag
- Actavis totowa llc
- Aurobindo pharma ltd
- Cadista pharmaceuticals inc
- Invagen pharmaceuticals inc
- Mutual pharmaceutical co inc
- Mylan pharmaceuticals inc
- Orit laboratories llc
- Pliva inc
- Ranbaxy laboratories ltd
- Sandoz inc
- Vintage pharmaceuticals inc
- Watson laboratories inc
- Mcneil pediatrics
-
Cyclobenzaprine Abuse and overdose
Cyclobenzaprine may enhance the effects of other central nervous system depressants, such as alcohol, barbiturates, benzodiazepines and narcotics. According to the DEA, abusers often combine cyclobenzaprine with these depressants to produce or enhance psychoactive effects. Though it is not a controlled substance, the DEA has recorded anecdotal reports of use to induce euphoria and relaxation.
Though rare, deaths can occur from cyclobenzaprine overdose, especially in the case of multiple drug ingestion. The FDA recommends that doctors contact a poison control center for current information on treatment for an overdose, as the management of a case is complex.
The most common manifestations associated with overdose are drowsiness and an abnormally rapid heart rate (tachycardia). Less common effects include body twitches (tremor), the loss of control of bodily movements (ataxia), hypertension, agitation, slurred speech, nausea, confusion, dizziness, hallucination, vomiting and coma. Rare but critical effects include cardiac arrest, chest pain and seizures.
Cyclobenzaprine Drug testing
A 2011, a double-blind randomized placebo-controlled study published by The Journal of Rheumatology found that the drug may also be useful in treating those with fibromyalgia sleep better. A 2016 drug used to deliver cyclobenzaprine into the body of fibromyalgia patients was recently halted during trials. Other drugs using cyclobenzaprine are also being tested to treat fibromyalgia, though. The current form of cyclobenzaprine is not approved by the FDA for the treatment of fibromyalgia.